Few FDA approved drugs have a reputation as controversial as Ketamine. This reputation is well earned. Originally developed in the 1960s as a short-acting anesthetic for battlefield use, in recent decades it has become notorious as a date-rape drug (‘Special K’)*, a club drug (‘Vitamin K’) and for its use in veterinary medicine (‘horse tranquilizer’).
However, I venture to bet that Ketamine is about to be rehabilitated for legitimate human uses. Here is why.
The reason for this belief is a most severe crisis in mental health and our approach to treating mental illness. It is not polite to say this, but given the gravity of the situation it needs to be said: It’s not working out. Not really.
Certainly a strong statement, but this sobering reality is becoming increasingly apparent. Every year, upwards of 10 million people experience a major depressive episode in the US alone. The number of people who never see a professional – and are thus never diagnosed – is likely much higher. Each of these episodes can be expected to last for months to years and is characterized by utter misery; a substantial number is terminal (the number of suicides in the US outnumbers the number of violent non-self gun deaths by about 3:1). Currently available “antidepressants” (a term I would use only in quotation marks, as most struggle to beat placebo except for the most extreme cases and might appear statistically more effective than they actually are) – these days usually a selective serotonin reuptake inhibior (SSRI) – can be expected to help one in ten people, and only after a trial period of 4 weeks to several months. Of course, if the depression happens to coincide with an underlying bipolar tendency, treatment with an SSRI will likely trigger a dysphoric mania. In other words, one will never reach the end of the interval that the SSRI needs to take to work (if it ever does). Instead, one will – at best – need to be hospitalized. So-called “treatment resistant depression” (in reality, depression that didn’t respond to treatment with a few SSRIs or SNRIs as MAO-inhibitors and tricyclics have largely fallen out of favor due to their side effect profile) is either allowed to take its course (with devastating consequences for the individual) or treated with electroshock therapy (ECT). ECT is remarkably effective in addressing this kind of depression, but the “side effects” (more aptly called treatment effects) like deleterious memory loss are a steep price to pay.
This state of affairs is obviously unacceptable. The good news is that it is increasingly being recognized as unacceptable. The National Institute of Mental Health (NIMH) recently announced that it would no longer fund research based on diagnostic criteria as outlined in the DSM. Psychiatric disorders are the only medical conditions that – for historical reasons – are diagnosed entirely based on subjectively reported symptoms. Doing this for any other condition, e.g. cancer or infectious diseases would obviously be absurd. Molecular biology has seen to that. In the 21st century, this simply will no longer do and the NIMH is essentially willing to start over from scratch.
Enter Ketamine. When Ketamine was used as a battlefield anesthetic in Vietnam and the first Gulf war, it was anecdotally noted that wounded soldiers such treated developed far fewer cases of PTSD than soldiers with similar injuries that were treated with other anesthetics. A couple of years ago, systematic studies showed that the vast majority of patients suffering from major depressive disorders made a rapid recovery when given a low, sub-anesthetic dose (most studies show a dose of 0.5 mg/kg to be effective) of Ketamine.
The clinical effectiveness of Ketamine in these scientific reports sounds too good to be true, particularly when compared with anything else on the market. The effects take hold within days (if not hours, compared with weeks to months for SSRIs), they seem to work for most people, there seem to be few discernible side effects (bladder issues seem to be a concern, but mostly at “recreational” doses and frequency of use) in stark contrast to – for instance – ECT), and it seems to be equally effective in the treatment of bipolar depression (which is notoriously hard to treat).
So what is the catch? Given the crushing disease burden inflicted by major depressive disorders, the question why this treatment is not readily available arises immediately.
The issue does not seem to be primarily medical in nature. Ketamine *is* a dissociate anesthetic, so the immediate effects on the conscious experience are rather extreme. Based on reports from people who have received low sub-anesthetic doses of Ketamine, the Kantian a priori categories of space and time seem to unravel shortly after the injection. They report that it becomes obvious that shared reality is a construct – brought about by the normal operation of the brain – but that Ketamine suspends this normal construction process, allowing for different reconstructions of reality. At higher doses, the reports speak of “leaving flatland” and becoming aware of higher dimensional objects that only appear to be separate when projected onto a low-dimensional space (such as the one we commonly perceive). Whether these experience reports sound scary or intriguing, there is no question that these experiences do not last very long. Given the short half-life of Ketamine and depending on individual metabolism and route of administration (IM or IV), these dissociative effects last for an hour or two, not longer.
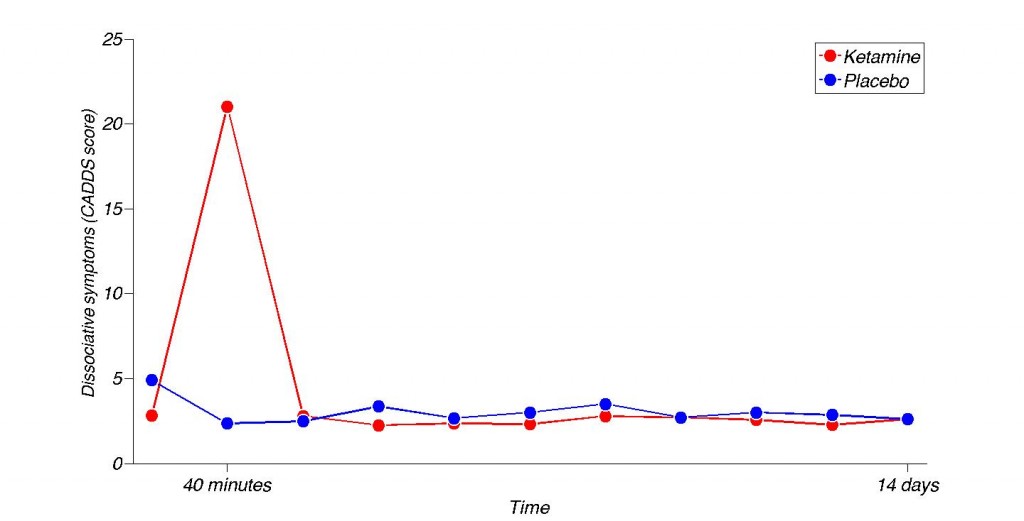
One of the most remarkable figures I’ve ever seen. Dissociative symptoms over time. x-axis is nonlinear. Differences at all time points other than the 40 minute mark are not significant. Adapted from Diazgranados, Nancy, et al. “A randomized add-on trial of an N-methyl-D-aspartate antagonist in treatment-resistant bipolar depression.” Archives of general psychiatry 67.8 (2010): 793.
It is also reassuring that the patients could *answer* the CADSS, so they couldn’t have been too far gone. Intriguingly, while there was no significant difference between placebo and ketamine group except for the 40 minute mark, *all* the mean scores of the placebo group seem to be slightly above the ketamine group. The CADDS features items like: “Do objects look different than you would expect?”. It is not inconceivable that, the experience properly calibrated the scale of the Ketamine group.
Obviously, there are no studies on long term effects in humans at this point, but similar studies on monkeys are encouraging. Animals which had received similar doses for long periods of time on a daily basis show that the dose has to be relatively high and the period of time relatively long to demonstrate impairment. Moreover, the doses involved in the treatment of pain are usually considerably higher, without reports of long term ill effects. To be clear: *Any* potential neurotoxicity is obviously cause for serious concern. However, all medical decisions involve tradeoffs. Depression in itself is increasingly linked to neurotoxicity. Moreover, the spectre of neurotoxicity can lurk where one least expects it, e.g. from antibiotic treatments. In addition, Ketamine seems to potentially *reverse* depression (or stress) induced brain damage via synaptogenesis. The moral of the story is that one should not embark on a course of medical treatment unless the expected upside (far) exceeds the expected downside.
Of course, there is a rub. More than one, actually. The two biggest and uncontested issues seem to be unclear mechanism of action as well as sustainability.
The first issue is that we do not really know or understand how Ketamine seems to bring about its antidepressant magic. Many theories are currently being explored in active research. Some of the hottest trails are NMDA antagonism, neurogenesis and dentritic sprouting. Personally, I believe there might be something to the notion that one is “growing a prefrontal forest”, strengthening prefrontal networks that are in turn able to better quench aberrant activity originating in evolutionary older structures (amygdala, limbic system, etc.) One way or the other, glutamate seems to be involved. While it may sound unsettling that we do not understand the mechanism of a treatment, this situation is far from unique. As a matter of fact, we do not understand the mechanism of action of *any* anesthetic drug. Similarly, there is plenty of evidence that even SSRIS don’t work the way we thought they do. There is mounting empirical support for the notion that the Serotonin action is largely incidental, and that neurogenesis is really behind their therapeutic effects.
The second issue – that of sustainability – is more serious. Curiously, the effects don’t seem to last. While Ketamine can rapidly pull someone out of a serious depression, the depression seems to return in time, requiring a “booster” shot to banish the demons again, even for a short while. The time until relapse is different from individual to individual, ranging from weeks to months, but it is intriguing that there is a time constant at all.
However, there are many chronic diseases that require daily administration of medications, including injections. In this regard, Ketamine isn’t even all that different from most other antidepressants, which are – more often that not – a pretty permanent deal. Many have to keep taking them, for fear of relapse. The real issue why these treatments are not more readily available seems to be economic in nature.
Ketamine is an extremely cheap drug, as it has been off patent for almost 40 years. Put differently, there is no money to be made here. The FDA is tasked with protecting the public from harmful treatments. Thus, the approval process is lengthy and costly. In reality, only a major pharmaceutical company has the financial resources to spearhead the approval of a drug. In the case of Ketamine, this is unlikely to happen, as these companies could never realistically expect to recover their expenses. To be clear, Ketamine already *is* FDA approved, but not for the treatment of depression. There are already some courageous pioneers who will administer Ketamine today (for a king’s ransom) in its off-label use for depression. This is not in itself unusual. Many drugs – once FDA approved – are prescribed for off-label uses. For instance, Modafinil was initially approved for the treatment of narcolepsy. Today, the vast majority of prescriptions are not issued by neurologists for narcoleptics, but rather by primary care physicians for people who feel a little tired – or simply because people want to use it. So in principle, Ketamine already is available for the treatment of depression, off-label. However, the overwhelming majority of psychiatrists is unlikely to touch a drug that is a PCP derivative and needs to be injected, no matter how effective. This problem is not unique to Ketamine. Once a drug has acquired a certain infamy, it is hard to change minds. For instance, Thalidomide is now being explored as an effective cancer treatment, precisely because its such a potent inhibitor of angiogenesis. But that’s a hard sell, given its historical record.
Where does this leave us? In an uncomfortable (as millions are suffering right now), but hopeful position. The evidence for the antidepressant effectiveness of Ketamine (for whatever, yet to be understood reason) is so overwhelming that quite a few pharmaceutical companies are feverishly working on Ketamine analogues and delivery methods (e.g. nasal sprays) as well as alternative NMDA modulators that *can* be patented and thus would be worthwhile to put through the highly demanding FDA approval process. Preliminary results are so promising that one can reasonably hope to have truly effective antidepressants available within another decade or so. If this happens, a mental health revolution will be at hand. And it will be sorely needed. Having rapidly acting and unequivocally effective antidepressants widely available and covered by insurance (akin to antibiotics) will make all the difference.
Note: There is no question that Ketamine is a crude drug when it comes to addressing the pathology that underlies depression. Nevertheless, it is a promising and encouraging start, not necessarily the end. Further drug development will need to hone in on the underlying biological target systems (which is why a mental illness classification based on biomarkers is so sorely needed). Moreover, it has not escaped my notice that this discussion has focused on psychopharmacological aspects of depression. There are other aspects that are social, psychological and nutritional in nature, among others. Etiology is likely complex. Breakdown in social coping structures? Sedentary lifestyles? Overfeeding? Intense and chronic stress? Extreme social competition and comparison? Sleep deprivation? Light pollution? Hormone disruption? There certainly is a discussion to be had about these aspects, but not now. It will take a while for research to disentangle these causal links. Meanwhile, it is important to lighten the burden of disease. Thus, the focus was deliberate and we will save a deliberation of other factors for later.
On a final note, it is quite unsettling that virtually all truly effective treatments for mental disorders (e.g. Lithium, ECT, Ketamine, etc.) and psychoactive substances in general (e.g. LSD, Benzos, etc.) were discovered entirely by chance, by pure serendipity. Conversely, all mental health treatments *designed* to do a certain thing, based on our current understanding of the nervous system (e.g. SSRIs, but not just SSRIs – one can always do worse) basically failed to deliver. This suggests that we do not currently understand it very well. Recognizing this should break a lance for pioneering (some call it basic, but there is nothing basic about it) neuroscience research.
PS: This is another installation in an ongoing series on how language really does matter. Most people suffering from depression would reasonably turn to antidepressants, not dissociative anesthetics for help. But just because marketing calls them that doesn’t make it so (whatever one’s position, they are on average so ineffective that a vigorous debate whether or not they are more effective than placebo is even possible. A debate we didn’t see regarding the effectiveness of penicillin. Regardless, there are so many vested interests involved here that the debate is likely to go on. So it is certainly premature to write “Listening to Ketamine” even as people are sick of listening to overhyped BS. Yet, the suffering of the suffering is so severe that I remain hopeful that reason will prevail in the struggle to make depression history. The notion to have effective antidepressants available is a powerful one). As it turns out, the antidepressant effects of some dissociative anesthetics are in all likelihood much more potent than that of current “antidepressants”. Go figure.
Be it as it may, it is downright scandalous to have people suffer every day, some of them killing themselves and have a safe solution (at the right dose) readily available, yet not allow it to be used. That this is even a possible – and ongoing – state of affairs does not instill confidence in the way things are in general. Downright scary, actually.
Update: The story has now hit the mainstream. Also, there is now solid evidence that repeated low dose administration of Ketamine seems to keep depression at bay, akin to maintenance ECT and without mounting side effects.
Update: In the piece, I expressed surprise at the fact that patients have not been more forceful in advocacy and outreach, demanding the FDA approval of this treatment on an emergency basis. This now seems to be happening. The website also compiles a – growing – directory of health care providers willing to administer Ketamine infusions. Given how bad the suffering can be – note this case of a woman enduring 273 (mostly bilateral) ECT treatments – without an appreciable effect on the depression, but dramatic and sustainable effects from low-dose Ketamine infusions on a maintenance schedule every 3 weeks. Note that dosage seems to be *critical*, with a very narrow therapeutic range between 0.4-0.6 mg/kg.
*It is possible that Ketamine acquired this reputation somewhat unfairly, as legislators might have confused it with the date-rape drug GHB when passing emergency legislation in August 1999 (classifying it as a schedule-3 substance in the US). Interestingly enough, GHB is now legally available as a drug for narcolepsy, Xyrem.
You referred to a place in NY and comment, parenthetically: “for a king’s ransom”. I checked the site and it’s $480 per treatment. That’s it? Are you kidding me? I’d pay many times that amount if it lifts depression in the way that has been described. I’ve paid many, many times that for therapy, psychiatrists, and of course, the crude and ineffective SSRIs and SNRIs themselves. $480, even if I have to do it 10 times, is a bargain.
I’m used to academic salaries 😉
One man’s “king’s ransom” is another man’s chump change. I think it is now upwards of $500 per treatment, and there is no chance in hell that insurance will cover it, so not everyone will be able to afford this. There are also a few other places around the country, so you might want to shop around for the best deal. The one I referenced has impeccable credentials.
As to whether it is worth it depends on one’s individual cost/benefit analysis. The efficacy of the treatment itself – according to the literature – is not in question.
If you decide that it is worth a shot and go that route, please report back how it went.
As I’m currently writing an essay on the efficacy of ketamine in depression, I thought it was so strange to not see it used in clinical setting, as Berman already showed the positive effects in 1999 (and research goes back even further, to 1959 where Crane first posed the NMDA receptor as a valid target). Your arguments make it very clear to me why it never happened and makes me even more convinced that the current system is not at highest efficiency. Though it is clear why the rules are how they are, they are far from optimal.
One side note on your comment on designer drugs: SSRI’s where developed in the 70’s as I recall correctly, when knowledge of system neurobiology was even a fraction of what we have now. Arguing from a mono-amine hypothesis, SSRI’s made a lot of sense and they do help a select group of patients. However, it is abundantly clear with the knowledge we have now that SSRI’s are far from optimal. My point is that I feel you are implying that SSRI’s are fairly new when they are not, and the body of evidence on the workings of SSRI’s is ever growing; I feel it is an exaggeration of the situation.
@Gerbrand: Thanks for the thoughtful comment. I don’t mean to appear like I’m picking on SSRIs. It’s just what most people are familiar with. And you’re right. They were a deliberate modification of the tricyclic concept, a long time ago. But that doesn’t mean that this isn’t still the case. New SSRIs are still coming to market (e.g. Viibryd as late as 2011) or are still in the pipeline. Each of them has a particular receptor binding profile, so this is not necessarily irrational if one believes that the design principle itself is sound. Which is the monoamine hypothesis, which is indeed quite old (maybe I should have emphasized that, but the piece is mostly about Ketamine, not SSRIs and was getting too long as is). Yet, other than Ketamine – which is even older – until very recently there really was nothing else of note in the pipeline (most alternatives struggle to beat placebo, even in the published literature, e.g. http://www.sciencedirect.com/science/article/pii/S0924977X05001392, to say nothing of file drawer effects). Only game in town. The way of looking at it has changed in recent years, *due* to the uncontroversial success of Ketamine in research trials, towards NMDA, neurogenesis, etc. But there yet has to come an approved, designed drug from that. I remain hopeful.
In terms of systemic solutions: Yes. It is important to recognize that demonization of any of the players (e.g. the FDA, the drug companies, etc.) is not helpful. They are all doing what they are supposed to, given the current system. It can be argued that the system itself is not conducive to those suffering from depression at this point in history, as all the incentives are misaligned with the interests of the patients (fast, safe, effective and affordable treatment).
HI – This is an interesting look at antidepressants you have here! I was trained in the 70’s to do the human, psychological side of evaluating proposed drugs. At that time there was more basic and university-based research in the US, it seems to me, and less of a corporate profit-motive based doorway to answering these questions. I think research in how to solve the problems of psychiatric disorders really needs to be done by government- or university/society- based funding. Otherwise we have this hamster wheel of meds that [seem to] help a few more people than placebo and have to rely on advertising agencies for a boost into public approval, until the patent runs out and they are “improved” for another round of patent protection, and again rely on advertising to increase the market – instead of just working. And as you say, we keep coming up with drugs to treat subjective disorders we haven’t really defined yet (DSM V aside). Maybe we need internet tiny-funding sites for some basic research proposals!
While there is (still) considerable research on depression within academia (most funded courtesy of NIMH), you are right about the business model.
We have seen the rise of direct-to-patient advertising of antidepressants, complete with appeals to ask one’s doctor http://www.youtube.com/watch?v=OTZvnAF7UsA and simplistic “chemical imbalance” models http://www.youtube.com/watch?v=6vfSFXKlnO0
Consequently, people go out and do ask their doctor for these medications. Mostly primary care physicians, actually. These days.
The model does work economically. I’m not sure if it works equally well for the patients.
Hey Dr. W–
Really cool to see more people talking about the potential benefits of ketamine. I went to a talk in an unusual venue last summer given by a Yale professor who was talking about the psychiatric benefits of ketamine and similar drugs, and there are a number of issues that were discussed there which I haven’t seen in this post– possibly because they are dubious in nature, or maybe you were unaware or just chose not to include them to avoid tl;dr.
-I guess the first thing to bring up, responsibly, is that ketamine itself is somewhat inappropriate for clinical use because it has high abuse potential. Most drugs which cause hallucinations are not particularly addictive, but ketamine unfortunately is. I believe tolerance also builds up quickly. All the more reason to fund research into developing derivatives/ analogues.
-in addition to its role in depression and bipolar, ketamine has been used pretty heavily in schizophrenia research. eg, http://yaledailynews.com/blog/2013/02/26/study-pinpoints-schizophrenia-causing-receptor/ Now one thing I remember from this talk I went to is that while administering ketamine caused an increase in the positive symptoms of schizophrenia (hallucinations, etc), there is a ketamine-like substance (I forget exactly where its mechanism of action on the NMDA receptor is, but I feel like it might have to do with the glycine receptor) which strongly REDUCES the negative symptoms– the ones that are notoriously most difficult to treat. In fact, straight-up ketamine will reduce negative symptoms of schizophrenia like lack of affect and catatonia. of course this line of thinking starts to sound like the medical marijuana debate– “yeah man herbs will cure everything, they just don’t want you to know, etc, etc”
-I agree with the problem with the system behind drug approval. Why is the industry so privatized? If the NIH funds research, where is the funding for clinical trials? Or drug production? There’s a crazy shortage of doxycycline right now simply because manufacturers failed to properly anticipate demand/profit potential. http://www.cdc.gov/std/treatment/doxycyclineShortage.htm Is there a reason basic pharmaceuticals cannot or should not be funded by the government?
I have been getting Ketamine shots by my pdoc for a couple months now. I can say, this is the ONLY thing that has given me a glimmer of hope, a chance to live my life again! I have been on SSRI’s, SRNI’s, MAOI’s, and have had several ECT treatments. Even the ECT treatment did not work as well as these shots. (Except wipe out my memory about 80% around the time of treatment).
I have had 5 injections. The first lasted a week, and ones after last about 2 weeks. They advise i get an injection when i FIRST start feeling like i am going down, not to wait till i cant get out of bed down.
Im so excited SOMETHING has finally given me hope, and my life back. I wonder about the side effects, but honestly the way i was going i surely woyld have ended up commiting suicide sooner or later because nothing was offering relief.
I get my shot in the office, they monitor me, i must have a ride home and thats it. It is a little uncomfortable having these weird ‘trips’ in my Dr.’s office, but it only lasts about an hour or two.
I’ve been taking ketamine and found life as we know it is in fact a computer program
Is there any experience with intranasal application of Ketamine? It´s easy, it´s cheap and anyone can use it by himself, starting with tiny doses and slowly going up.
There are several companies working on a nasal delivery system. Obviously, that would be best in terms of feasibility for all involved. It is my understanding that there are (still?) issues with efficacy. Route of delivery does seem to matter. We’ll see. But this is certainly an exciting prospect for the future. It also does solve the issue of profitability, as the delivery system itself *can* be patented.
Having read about some very exciting cases of OCD being controlled with Ketamine, I have become very interested in trying it to treat my own very debilitating OCD. I also have narcolepsy and cataplexy. Does anyone know if Ketamine can be used by narcoleptics? I’d appreciate any info. THANK YOU
I am a founder of one of the first ketamine depression clinics. Since this is not an advert I am staying anonymous so my points will be considered more objectively.
1. Ketamine is in the exact situation that Lithium was in for the exact same reasons, and the solution is the same – the government paid for the FDA studies in the interests of the public. That is a little difficult now that the FDA is largely funded by Pharma since the 1990’s. Yes, it is bad to demonize except when you’re dealing with a demon.
2. There are over 1,000 successful ketamine patients at private clinics now. At ours, we have as patients one psychiatrist, two other physicians, two psychologists and two psychiatric nurses. The people in the know with resources are already getting the treatment and finding personal success.
3. The rates of anyone are not a king’s ransom. With the costs largely fixed, and small volumes of patients, the per treatment cost is quite high. The cost of the meds is a nit.
4. Clinics have achieved sustained remission rates. Most people do not understand how ketamine works on depression. It is two-fold. First, there is the neurogenesis that is commonly known. Second, ketamine at the right dose rate dramatically lowers ego boundaries, allowing the patient to understand their own unconscious motivations. One or our patients called it affectionately an “emotional enema” – nobody leaves our treatment rooms with dry eyes. The combination of the action of ketamine on brain structure plus appropriately targeted psychotherapy to support the patients’ growing awareness results in lasting improvements in all areas of the patients’ lives.
Thanks for the well-considered points and thanks for providing thousand-fold relief to people that the system basically has otherwise given up on. To clarify:
1. While ketamine is in the same position as lithium patent-law wise, there is an important difference: Ketamine has the added stigma of (growing) recreational use and being a schedule III (in the US) and class B drug (in the UK). To my knowledge, lithium is not used recreationally, nor is a controlled substance. So few psychiatrists are (in my experience) willing to go anywhere near it.
2. “King’s ransom”: Deliberate hyperbole to shame the powers to be (not the clinics). From the perspective of the sufferer, it can be considered a scandal that garden variety – but largely ineffective – SSRIs are routinely covered by insurance while they won’t touch ketamine with a 10 foot pole. So from the perspective of the afflicted, the difference in cost is considerable. Particularly given the fact that – as you point out – ketamine itself is dirt cheap.
What I don’t understand is this: Why is the volume of patients low? Given the prevalence of depression, the effectiveness of ketamine and the ineffectiveness of alternatives, I would expect patients to beat down your door. Is it conceivable that price keeps them away? Not everyone can afford the current rates.
The truth that almost any substance has the potential for abuse does not mean that the average person would be prone to abuse anything. Fast food has the potential for abuse, yet most people simply consume normal amounts of it simply because they are hungry. As far as ketamine is concerned, I would just like to know if my brain still has the capacity to enjoy any aspect of life. Is there a chance that I can feel “normal” again? For just a few hours or days, I’d like to feel like Noah felt when the rain finally stopped!
Let’s keep the talking going…
As soon as it is found to be the most effective treatment…. cheap too… compare ect costs on a maintain program…. and when that happens everyone will jump on, driving cost down….
We need this now…. I need this now,, nasal studies need to incorporate sketamine and get rid of the psycho effects…
One can self administer morphine for cancer pain…..what about my pain,, , is it less important than anothers pain… because it is a mental illness
After having read a great deal of what’s been published about ketamine, and not having the funds to go the legal route, I ended up buying some from a recreational user and administering myself, using the dosage published in most scientific trials (0.5mg/kg IM). I don’t know how to explain the difference without resorting to cliche, but I cried the day after my first injection – not out of pain, but out of the cessation of pain. I don’t feel high or manic, which was a fear. I feel like I assume “normal” not-depressed people feel. It allows me to feel and react and function like a living person and I have hope again, which I had lost in the constant stream of therapists telling me I wasn’t trying to get better and pills that just didn’t work. With diagnoses of major depressive disorder and PTSD, life wasn’t worth living. I have three suicide attempts under my belt. Ketamine changed all that. I just wish I didn’t have to break the law to get to this point.
Wow, This is the first “sober” discussion involving professionals and treatment recipients (potential and current) together, that I think I’ve ever encountered. Incredibly refreshing. I believe the impending critical status regarding the gross and pervasive lack of efficacy with depression drugs was very well characterized by OP, Lanscap. Almost poetic, I must say. I’m afraid to confess, that I’m afraid to admit, how pervasive the seemingly apathetic—or perhaps more accurately, indistinct—acknowledgement of the simple fact that many patients struggling with depression are not being treated with any reasonable efficacy by the numerous drugs on the market, and claimed to make a difference. These “seemingly” magic pills have been enthusiastically promoted by pharm companies to such a magnitude that one can hardly escape the din of side-effects disclosures recited ad-nauseum on TV commercials.
It sometimes feels like your being told “well, you know SSRIs really don’t provide much more than +/- 30% efficacy, maybe, so… Would you like to try ‘SSRI#34′ and see if it helps better this time?;’ every six months or so. Am I the only person recognizing the irony in this? I’ve been hearing this for 15 years, from probably 20 different Pdocs.
The potential for relief that low dose Ketamine Infusion offers is so exciting, that I find myself fantasizing of ways to overcome the prohibitive “king’s ransom” and finally take the next exit off this gridlocked highway of suspended animation. Unfortunately I’m unable to even come close to affording treatment, as my illness has effectively relegated me to “disabled” status, with healthcare resources restricted to Medicare.
I once dreamt of convincing Medicare to cover treatment by somehow making the case that the drug is FDA approved, just not for depression. I made some plea regarding compassionate mandate or some such nonsense. What is so absurd, is the cost of regular Lithium levels, liver panels and the cost of the useless drugs I currently take—that Medicare covers every month—would pay for the ketamine and a nice massage and steak dinner. And I’d feel so much better.
I do have hope that the current Naurex candidates that are fast-tracked in phase 3 trials will make it to market and prove as efficacious as is likely. I’d just like to be able to work with Ketamine IV in the meantime, and hope to avoid the godforsaken hospital for the 11th time and maybe actually get out of the house.
I believe that the population of those Dx with depression deserves advocacy and a much louder voice, but unfortunately only a tiny percentage of us has the wherewithal to gather their energy, stand up and make some noise, it seems. Unfortunately the very nature and disposition of depression is contrary to such potency. Who can lend us their resilience and stamina, to help create a much needed awareness before the levy breaks? Perhaps a petition at Change.org might “grease the wheel?”
You guys are great. Thanks!
Hey,
I’d like to point out the most of the “expensive” treatment options for ketamine are due to the IV route of administration. However, I have been receiving intramuscular ketamine injections for over two years at a practice in NYC that charges $250/ injection, which is certainly better than the normal $500 price tag. I can personally attest to the quality and professionalism of this practice. The doctors name is Edward Fruitman, and I discovered his practice, Trifecta Health, through this video on youtube:https://www.youtube.com/watch?v=3W6q3tTaSbY Seriously, good people at that practice. I hope this helps somebody here, it certainly has changed my life. Good Luck!